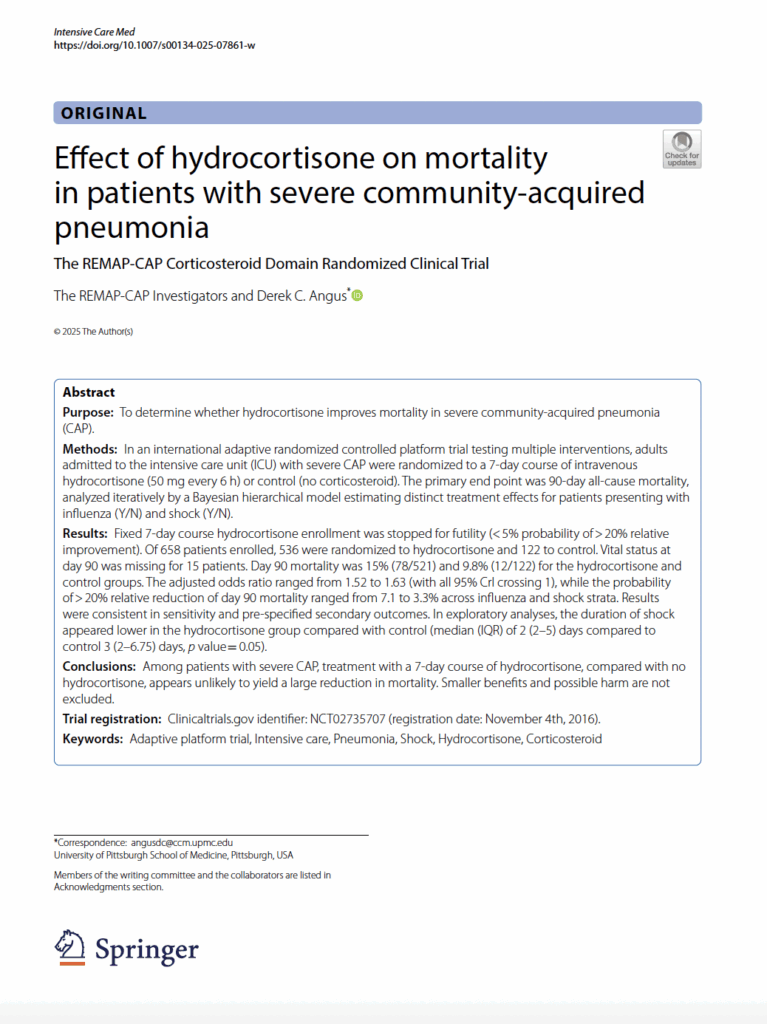
BACKGROUND
Corticosteroids may reduce mortality in patients hospitalized with severe community-acquired pneumonia (CAP). Possible benefits include amelioration of organ damage secondary to excessive host inflammatory responses via their anti-inflammatory properties, or mitigation of septic shock via their effects on the renin–angiotensin– aldosterone axis. Corticosteroids lowered mortality in patients with severe COVID-19 pneumonia, in a recent study of severe CAP, and in a post hoc analysis of CAP patients in a larger trial of steroids for septic shock. A recent guideline statement now recommends corticosteroid administration for severe CAP. However, other studies yielded inconsistent results, corticosteroids carry known side effects, and uncertainty persists regarding the type and dose of corticosteroids and whether treatment should be given broadly or to particular subgroups of patients. REMAP-CAP is an ongoing international platform trial (NCT02735707) designed to evaluate treatments for patients with severe CAP in pandemic and non-pandemic settings. The REMAP-CAP investigators previously reported that hydrocortisone appeared to be beneficial in patients with severe COVID-19, administered either as a fixed-dose 1-week course or titrated depending on the presence and duration of shock. REMAP-CAP also contains a corticosteroid domain for non-COVID-19 pneumonia, where patients were randomized to one of several corticosteroid strategies or control. On December 6th, 2023, the platform ceased randomization to one of the corticosteroid strategies, fixed-duration hydrocortisone, on the recommendation of the Data Safety and Monitoring Board (DSMB) after that arm triggered a pre-specified stopping rule for futility compared to control (no corticosteroid). Data were locked after the last patient completed follow-up for the primary end point and the results are presented here.
METHODS
In an international adaptive randomized controlled platform trial testing multiple interventions, adults admitted to the intensive care unit (ICU) with severe CAP were randomized to a 7-day course of intravenous hydrocortisone (50 mg every 6 h) or control (no corticosteroid). The primary end point was 90-day all-cause mortality, analyzed iteratively by a Bayesian hierarchical model estimating distinct treatment effects for patients presenting with influenza (Y/N) and shock (Y/N).
RESULTS
Fixed 7-day course hydrocortisone enrollment was stopped for futility (< 5% probability of > 20% relative improvement). Of 658 patients enrolled, 536 were randomized to hydrocortisone and 122 to control. Vital status at day 90 was missing for 15 patients. Day 90 mortality was 15% (78/521) and 9.8% (12/122) for the hydrocortisone and control groups. The adjusted odds ratio ranged from 1.52 to 1.63 (with all 95% CrI crossing 1), while the probability of > 20% relative reduction of day 90 mortality ranged from 7.1 to 3.3% across influenza and shock strata. Results were consistent in sensitivity and pre-specified secondary outcomes. In exploratory analyses, the duration of shock appeared lower in the hydrocortisone group compared with control (median (IQR) of 2 (2–5) days compared to control 3 (2–6.75) days, p value = 0.05).
CONCLUSIONS
Among patients with severe CAP, treatment with a 7-day course of hydrocortisone, compared with no hydrocortisone, appears unlikely to yield a large reduction in mortality. Smaller benefits and possible harm are not excluded.